Sin comentarios
Suscríbete a Bebés y más
Lola Rovati
@Lolarovati
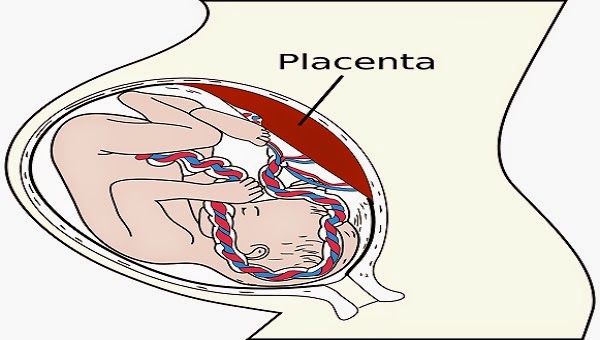
La placenta es un órgano que se forma dentro del útero durante el embarazo y que ayuda a nutrir al bebé y a filtrar el exceso de deshechos que se van generando durante los meses de gestación. A medida que avanza el embarazo, la placenta va evolucionando, y en su evolución la placenta puede clasificarse en cuatro grados de madurez: 0, I, II y III.
Durante el segundo y tercer trimestre del embarazo la placenta presenta cambios fisiológicos que permiten esta clasificación numérica por estadios o grados en base al aspecto de las calcificaciones intraplacentarias.
Desde el punto de vista ecográfico hay varias clasificaciones, pero es la de Grannum de 1979 la más conocida, y se clasifica en:
 Los tabiques de ambas partes de la placenta ya confluyen y se fusionan entre sí. En el interior de los cotiledones placentarios (los ovillos que forman las vellosidades coriales) se observan zonas de calcificación y degeneración.
Los tabiques de ambas partes de la placenta ya confluyen y se fusionan entre sí. En el interior de los cotiledones placentarios (los ovillos que forman las vellosidades coriales) se observan zonas de calcificación y degeneración.Grados de maduración de la placenta
Cuando una placenta se presenta en el grado II o III antes de la semana 34 puede decirse que está envejecida prematuramente. Ya hemos explicado cuándo se dice que hay placenta vieja o hipermadura.
Esto podría llevar a pensar que el bebé desarrollara una restricción en su desarrollo por insuficiencia placentaria, ya que esta insuficiencia produce, en el feto, hipoxemia y déficit nutricional. Esto último es causa de retraso de crecimiento intrauterino, por ello es importante realizar un adecuado control prenatal, especialmente en la etapa final del embarazo.
El desarrollo de la placenta suele seguir un patrón uniforme hasta las 20 semanas.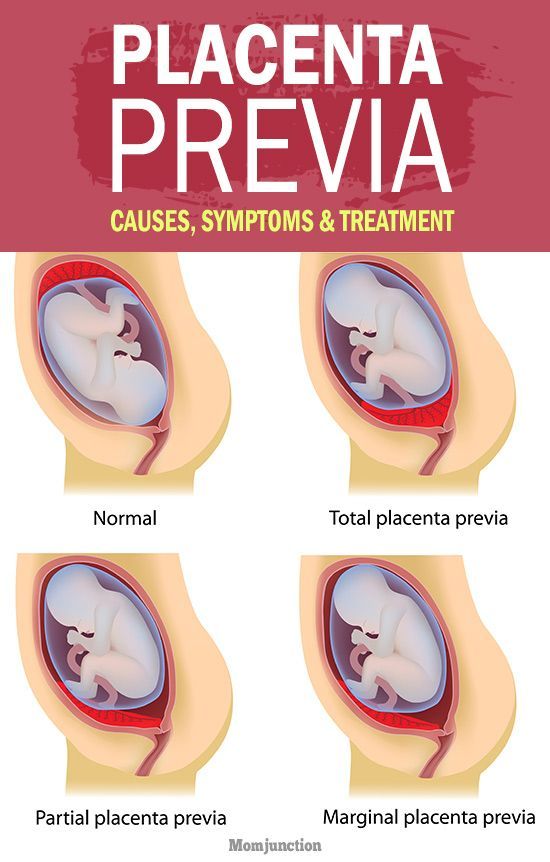 Luego, su volumen aumenta según las necesidades del feto. El retraso de crecimiento intrauterino asimétrico suele producirse por procesos que comienzan después de las 24 semanas y que llevan a insuficiencia placentaria, con envejecimiento prematuro.
Luego, su volumen aumenta según las necesidades del feto. El retraso de crecimiento intrauterino asimétrico suele producirse por procesos que comienzan después de las 24 semanas y que llevan a insuficiencia placentaria, con envejecimiento prematuro.
Aplicando la clasificación de Grannum, se asocia placenta grado II o III antes de las 34 semanas en el 60% de fetos con retraso de crecimiento y grado I o II antes de las 30 semanas en el 80%.
Suscríbete para recibir cada día nuestros consejos sobre embarazo, maternidad, bebés, lactancia y familia.
La clasificación de Grannum (grados 0-3) es la más conocida; posteriormente otros autores, como los españoles de la Fuente y Olaizola, realizan otra clasificación (grados I-IV), que se correlaciona con la de Grannum, con los mismos criterios de diferenciación placentaria.
En definitiva, los grados de maduración de la placenta constituyen la clasificación que se puede emplear para determinar el momento evolutivo en el que se encuentra dicho órgano, y comprende desde el 0 o grado más joven al III, grado más maduro.
Se observan mediante ecografía y son importantes para el control de salud fetal en la recta final del embarazo.
En Bebés y más | La placenta es un depósito de defectos genéticos que ayuda al bebé a corregirlos o evitarlos
Temas
Madres y mujeres embarazadas de guardia! ¿Hablamos del grado de la placenta? Creo que casi todo el mundo ha escuchado que la placenta es el órgano responsable de la nutrición del bebé dentro del vientre de la mamá. Sólo que la placenta nace junto con el embarazo, en cuanto el bebé se fija dentro del útero, la famosa nidación.
El cigoto iniciado por un óvulo y un espermatozoide se multiplica y, desde el momento en que se fija, se divide en dos partes distintas: una mitad se convertirá en el bebé y la otra en la placenta, que es totalmente necesaria e indispensable para el crecimiento, la oxigenación y la alimentación del bebé.
La placenta tiene un aspecto similar al de un hígado de buey. Está lleno de vasos sanguíneos que reciben la sangre rica en vitaminas y oxígeno para el feto y la transmiten a éste a través del cordón umbilical, permitiendo así que el bebé se desarrolle correctamente. Pero la placenta tiene grados de madurez.
Los grados de la placenta pueden ser grado 1, grado 2, grado 3 y 0. Lo que determina estos grados es la madurez de la placenta, es decir, cuanto más alto es el número, más “vieja” es. El grado de la placenta puede determinar la cantidad de alimento y oxígeno que recibe tu bebé, así que digamos que cuando está en grado 1 puede nutrir y oxigenar muy bien al bebé sin ningún riesgo.
La placenta de grado 2 es la que puede permanecer durante más tiempo en un embarazo. Puede comenzar en torno a las 28 semanas y seguir hasta las 36, 37 semanas o incluso el final del embarazo sin ningún problema. El grado 3 es el máximo grado de madurez de la placenta, pero esto no significa que no esté supliendo las necesidades del bebé, sólo que está “cansada” y también puede significar que el parto está cerca. Recuerda que el grado 0 es el mejor de todos. Indica que la placenta no tiene signos de madurez y que el embarazo está bien.
El grado 3 es el máximo grado de madurez de la placenta, pero esto no significa que no esté supliendo las necesidades del bebé, sólo que está “cansada” y también puede significar que el parto está cerca. Recuerda que el grado 0 es el mejor de todos. Indica que la placenta no tiene signos de madurez y que el embarazo está bien.
Si el embarazo llega a su fin y el grado sigue siendo 0, puede ser una señal de que el embarazo está cerca de las 42 semanas. Pero eso no es todo, también puede indicar que la madurez de los pulmones no es completa, pero no es un problema. La mujer embarazada debe mantener la calma y hablar con su médico.
Placenta extraída en un parto normal, escenas fuertes para los que no les gusta ver sangre así que ¡cuidado!
He visto casos de madres con 30 semanas de embarazo y placenta grado 2, pero también he visto con grado 3, si este es tu caso no te preocupes, habla con tu médico para que te tranquilice. El embarazo suele producirse sin problemas incluso con una placenta de grado 3 en lugar de una de grado 2.
Yo misma tuve una placenta de grado 2 a las 29 semanas de embarazo y fui sin problemas hasta el final cuando ya estaba con una placenta de grado 3 a las 39 semanas. A medida que la placenta madura, el líquido amniótico le sigue y la madurez del bebé también contribuye a ello. Leí en algún sitio que el pulmón del bebé segrega una hormona cuando está maduro y esto puede acelerar la maduración del grado de la placenta al final del embarazo y por eso muchos embarazos llegan al grado máximo de maduración. Por lo general, el grado de la placenta no es motivo de preocupación.
Lo que puede adelantar un parto no es el grado de placenta sino el estado de la misma. Por ejemplo, una razón para posponer el parto, o para pensar en inducirlo, sería la calcificación de la placenta. Es cuando la placenta empieza a empedrarse o calcificarse (endurecerse) y entonces no le pasa nada bueno al bebé, lo que lleva al médico a hablar de parto. Pero ese es un tema para otro post…
Pero ese es un tema para otro post…
A las 34 semanas, el control prenatal es aún más cuidadoso y detallado, y si el US muestra un grado 3 a esa altura es necesario comprobar la oxigenación del bebé; si es buena, no hay problema. En el examen Doppler de las arterias umbilicales y de la placenta que normalmente se solicita en la fase final del embarazo es posible comprobar las condiciones de oxigenación.
¡No, al contrario! Cuanto más baja es la placenta, más joven es y mejor está haciendo su trabajo de nutrir y oxigenar al bebé. Si quieres tener un parto normal, un grado bajo de placenta en la fase final puede indicar que tardarás un poco más en ponerte de parto.
Es una placenta más gruesa de lo que se considera normal y puede estar causada por una pequeña calcificación unilateral, parcial o completa. Tiene las características como si fueran pequeñas piedras de sangre en toda su extensión. No es un caso alarmante, pero es necesario estar acompañado por un médico.
Tiene las características como si fueran pequeñas piedras de sangre en toda su extensión. No es un caso alarmante, pero es necesario estar acompañado por un médico.
Consejo importante: La mamá que da a luz una nueva vida necesita tener todas sus vitaminas al día. Un buen multivitamínico es esencial en esta fase de la vida y por eso Famivita ha desarrollado FamiGesta. FamiGesta es la única vitamina con metilfolato, la forma activa del ácido fólico. Puede obtener más información sobre FamiGesta aquí.
Ver también: Cordón umbilical y ombligo del bebé – Su función dentrodel útero
Foto: premasagar
Premature maturation of the placenta means the appearance of signs of maturity of the placental tissue before the gestational age, for which such changes are physiological. This condition does not manifest itself in any way and is detected on ultrasound screening.
Premature aging of the placenta is dangerous because the child will not receive adequate nutrition and oxygen.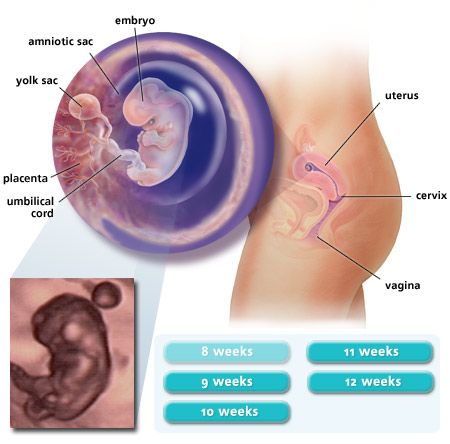 This can lead not only to fetal growth retardation, intrauterine hypoxia and premature birth, but also to the death of the child.
This can lead not only to fetal growth retardation, intrauterine hypoxia and premature birth, but also to the death of the child.
The placenta (from Latin Placenta – cake) is also called a children’s place, which is the link between the baby and the mother. It is this temporary organ that ensures the delivery of nutrition and oxygen to the fetus, and also protects it from external influences.
Placental tissue has a spongy structure. On one side, it is adjacent to the uterine wall, from where it receives blood thanks to common vessels, the other is connected to the child through the umbilical cord.
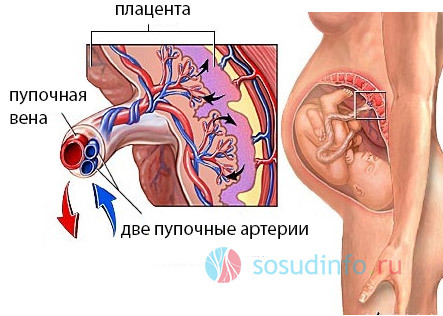
The child’s place plays the role of a barrier that prevents the mixing of the blood of the mother and fetus. Through it, fresh blood, enriched with vitamins and minerals, enters the latter through a vein inside the umbilical cord.
The metabolic products of the fetus – urea, carbon dioxide, creatinine – are excreted through 2 umbilical arteries.
The placenta synthesizes important hormones for the pregnant woman.
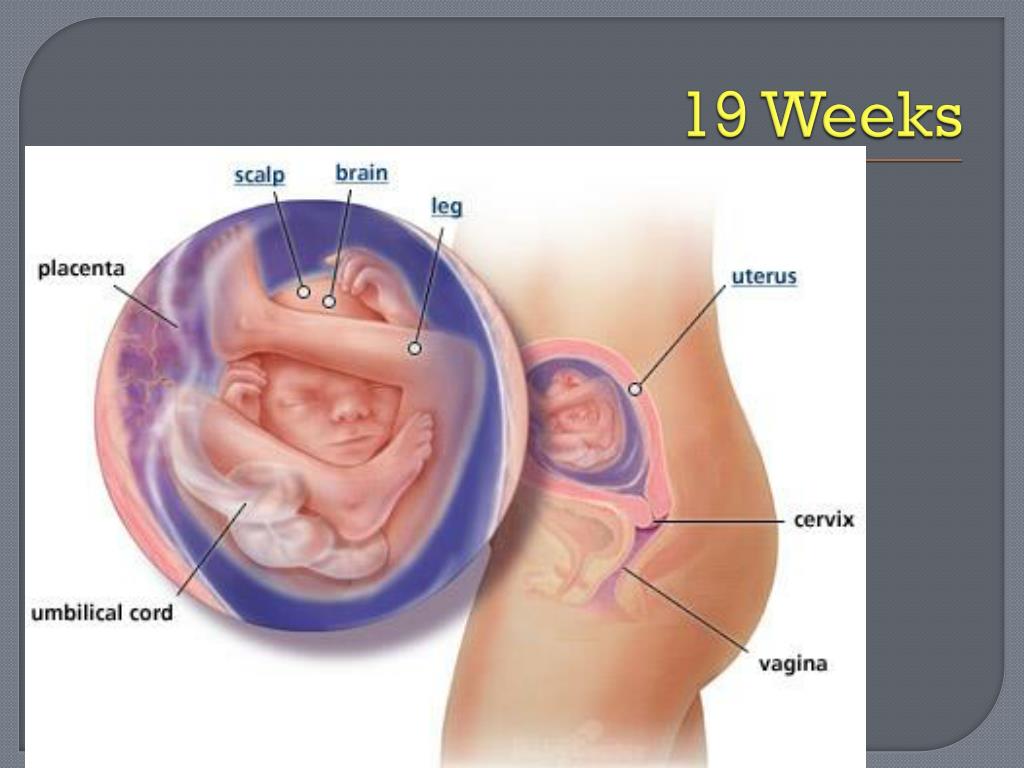
A week after ovulation, the fetal egg enters the uterus and is introduced into its wall due to the chorionic membrane, which literally grows into the endometrium by dissolving epithelial cells. At the site of attachment, a chorion is formed, which gradually transforms into the placenta, and by 14-16 weeks this process is completed. But the final form of the child’s place takes on only by the 20th week.
Until the middle of pregnancy, the young placental tissue increases and expands more and more, in the later stages it only adds a little in thickness.
The functionality of the placenta decreases along with the duration of pregnancy. It gradually develops its resource and grows old. At first, its membranes take on a wave-like shape, later point blotches appear in the placental tissue, consisting of deposits of calcium salts.
Further, these deposits increase, the sponginess is more and more smoothed out, giving density to the children’s place, which at the same time becomes thinner.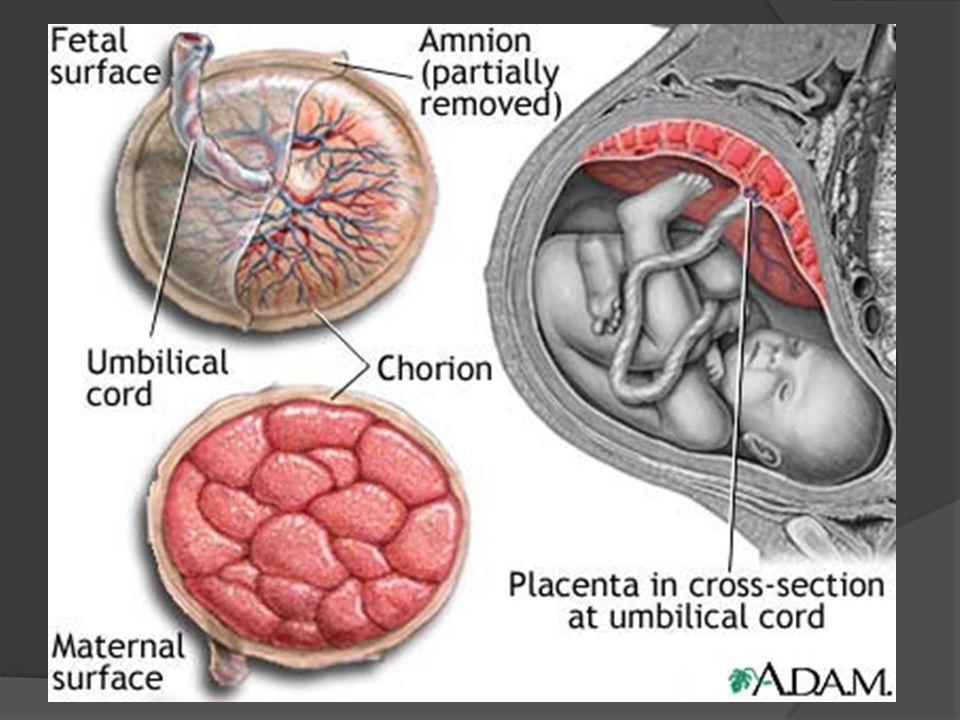 But all the described processes are physiological as long as they coincide in time with generally accepted standards.
But all the described processes are physiological as long as they coincide in time with generally accepted standards.
There are 4 degrees of maturity of the placenta, which replace each other at a time determined by nature. If these deadlines are met, the child is not in danger. Otherwise, with a more rapid “fading” of the placental structure, we are talking about early aging. During a remote consultation, our doctors will connect independent doctors to provide a second opinion, make a list of tests, and analyze the reasons.
The placenta during pregnancy matures in 4 stages, each of which has its own distinctive ultrasound signs:
|
The degree of maturity of the placenta |
Terms, weeks |
Peculiarities |
|
Zero |
up to 30 |
There are no inclusions, placental tissue is homogeneous, tends to increase in mass and volume |
|
First |
30-34 |
There are a small number of echogenic inclusions due to the compaction of the stroma, slight waviness of the chorionic plate. |
|
Second |
35-39 |
The waviness of the chorionic membrane is more pronounced, fragmentary thinning of the placental tissue is noted, its structure becomes denser, calcium deposits appear |
|
Third |
37 and more |
3 degree of maturity of the placenta is manifested by the tortuosity of the chorionic plate. The previously smooth structure becomes lobulated and looks like a cluster of round lobules with rarefaction in the middle. Calcium deposits are clearly visible. The size and exchange area of placental tissue are reduced |
We can talk about premature maturation of placental tissue if:

Such a development of events indicates a high risk of a functional deficiency of placental tissue and decompensation of the adaptive capabilities of the “woman-child” system.
Attention! Normally, the 3rd degree of maturity of the child’s place is noted almost before the very birth, in the last weeks, and sometimes days before the onset of labor.
The placental structure begins to age prematurely due to various reasons that can lead to increased work of the “woman-child” complex. The mechanism of early aging can be triggered by external and internal factors due to the pathological course of pregnancy.
Why does the placenta age early?
 With short-term gestosis, nothing threatens the child’s place, since the normal blood supply to the fetus is maintained due to the compensatory resources of the body. If toxicosis lasts a long time, accelerated growth of placental tissue begins, so it matures and ages faster;
With short-term gestosis, nothing threatens the child’s place, since the normal blood supply to the fetus is maintained due to the compensatory resources of the body. If toxicosis lasts a long time, accelerated growth of placental tissue begins, so it matures and ages faster; It is in the power of a woman to protect herself from many factors that are fraught with problems with a child’s place: stop drinking alcohol, smoking and be especially careful when taking medication. If you have any questions, please contact our doctors. At a remote consultation, they will select analogues of drugs, they will be in touch at any time of the day.
Aging of the placenta during pregnancy occurs faster under the influence of radiation, chemical, temperature effects in everyday life and at work. The likelihood of such an outcome is increased by factors such as:
Attention! Early aging of the placenta is more common in multiple pregnancies and hormonal disruptions.
Premature aging of the placenta in itself is not dangerous for the mother and child. It becomes a threat if the condition of the fetus worsens. It is important to understand that really serious deviations in the “age” of the placental tissue are cause for concern, since this organ is able to fully function even with partial damage or detachment.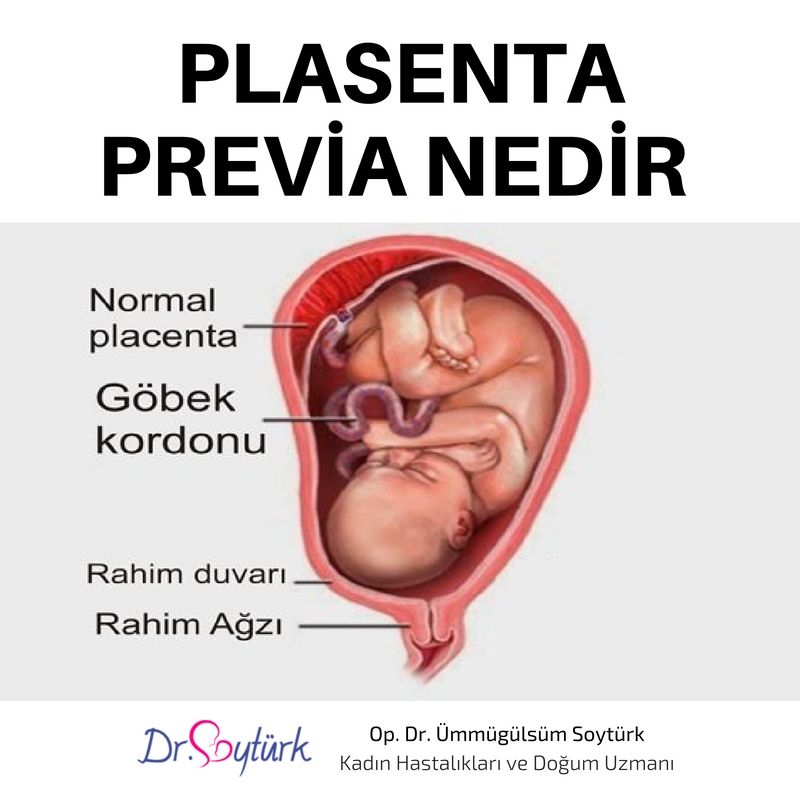
The alarm should be sounded in case of a clear lag in the development of the fetus. In order not to miss it, it is necessary to periodically do unscheduled ultrasounds.
Case study:
Ultrasound at 29 weeks showed signs of early maturation of the placenta. The woman donated blood for a coagulogram and platelets, according to the results of the examination, Curantyl was prescribed. Dopplerometry showed no abnormalities. The doctor recommended a second ultrasound in a month and assured me that complications were unlikely.
The symptoms of suffering in a child are as follows:
These symptoms are an indication for medical intervention with possible hospitalization, up to urgent delivery.
If signs of early aging of the placenta occur at 22-26 weeks of gestation, then the likelihood of significant developmental delay and intrauterine fetal hypoxia is very high.
With an early manifestation of the pathology, accompanied by dystrophic and sclerotic changes, early discharge of water and detachment of the placenta, as well as premature birth, are often noted.
Attention! In severe cases, intrauterine death of the child is not excluded.
If early aging of the placental tissue is detected at any time, the main pathology is treated, first of all, regardless of its type. To do this, drugs of various drug groups are used, including antibiotics, immunomodulators, steroids, cardiac drugs.
Specific therapy is aimed at improving the blood supply to the fetus. Antithrombotic, vasodilator drugs, amino acid complexes, hepatoprotectors cope with this task.
Of great importance are non-drug methods – dosed physical activity, a balanced diet, an optimal mode of work and rest.
Case study:
A woman at 36.2 weeks of pregnancy was diagnosed with “premature aging of the placenta of the 2nd degree.” The thickness of the placental tissue is 32 mm, multiple persificates. The development of the fetus corresponds to the gestational age, the blood flow is not disturbed, there is a single entanglement of the umbilical cord in the neck. Presumably, percificates and entanglement are a consequence of the transferred ARVI, which at such a time is no longer dangerous. This did not affect the child, since the blood flow and all parameters are normal.
What drugs are used for treatment?
+
The standard treatment regimen includes antispasmodics (No-shpa, Papaverine) to reduce uterine contractility, agents to improve microcirculation (Kurantil, Actovegin), vitamin complexes. If fetal hypoxia is suspected, oxygen cocktails may be prescribed to a woman.
What are the indications for emergency delivery?
+
The lack of effectiveness of the treatment and the presence of negative dynamics of the state of the baby.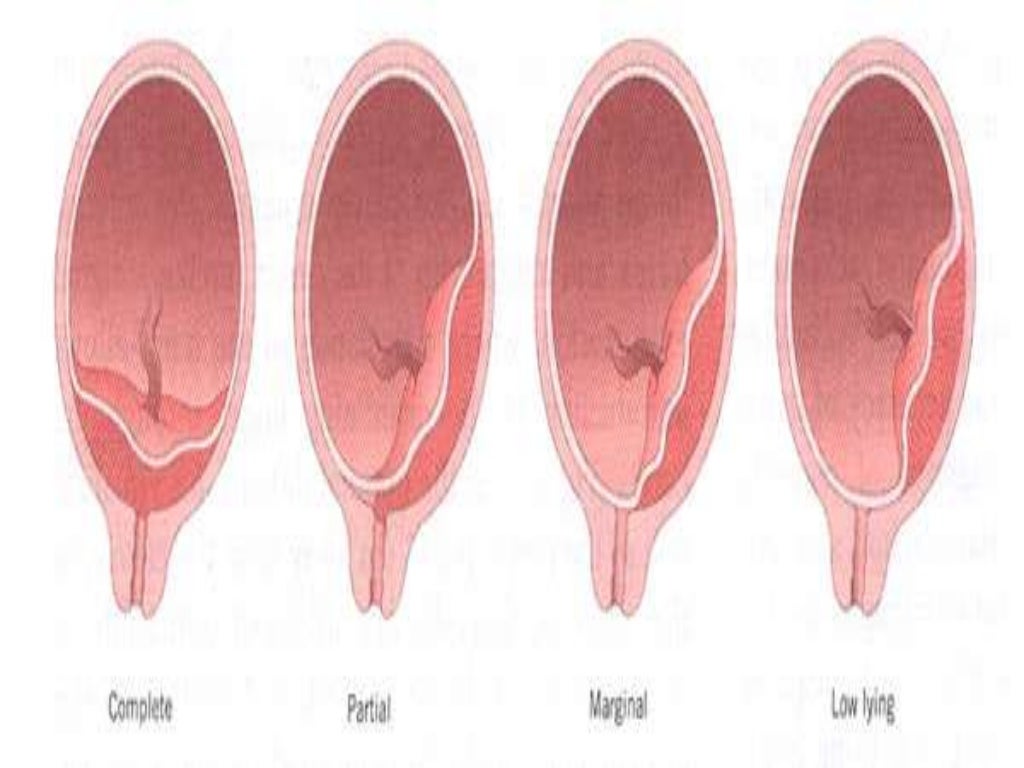
How many weeks of pregnancy is considered safe for an emergency delivery?
+
31-33 weeks. The indication may be a critical violation of the umbilical blood flow, CTG signs of oxygen starvation of the fetus, cessation of its growth, a sharp drop in the volume of amniotic water, as well as the presence of other conditions that threaten the health of the child.
Is it true that an old placenta can cause pregnancy to fail?
+
Yes, at maturity up to 25 weeks.
What tests are ordered to confirm the diagnosis?
+
Blood test for trophoblastic β-globulin, placental lactogen. If the level of these proteins is not reduced, then the placenta is functioning normally. However, these studies are not specific and are not significant diagnostic criteria.
What are the main ultrasound signs of an old placenta?
+
First of all, this is its thickening of more than 35 mm, the appearance of calcium deposits, increased waviness of the chorionic plate.
Premature aging of the placenta requires a strictly individual approach, taking into account the underlying disease. Subject to the timely detection and adequate treatment of pathology, the risk of placental insufficiency can be reduced and the pregnancy can be extended to a time that is safe for the birth of a baby.
We publish only verified information
Article author
Menshikova Maria Viktorovna
obstetrician-gynecologist
Experience 38 years
Consultations 1816
Articles 46
Specialist with extensive practical experience. He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
During pregnancy, a woman is concerned about many issues, but most of all she is interested in the time of delivery. This is usually associated with the fear of pain, any complications, and with the most important question – how will the birth end for the mother and child? All these fears are in vain. Modern obstetrics has vast experience in preparing pregnant women for childbirth and special monitoring of the course of childbirth, which makes it possible to timely diagnose complications from the mother or fetus and provide adequate assistance to both. Finally, methods have been developed by which a woman herself can contribute to the successful course of childbirth and reduce pain.
Modern obstetrics has vast experience in preparing pregnant women for childbirth and special monitoring of the course of childbirth, which makes it possible to timely diagnose complications from the mother or fetus and provide adequate assistance to both. Finally, methods have been developed by which a woman herself can contribute to the successful course of childbirth and reduce pain.
Pregnancy lasts an average of 280 days (40 weeks) from the first day of the last menstrual period. If you count 3 months ago from this date and then add 7 days, this will be the approximate date of delivery. For example: the last menstruation was on December 10, therefore, childbirth can be expected on September 17.
It is advisable to remember the day of the first fetal movement. Primiparous women feel it in the middle of pregnancy (20 weeks), and multiparous women a little earlier (18 weeks).
It will be possible to speak most accurately about the date of birth if the gestational age is established. It can be determined by the doctor by the size of the uterus, which correspond to certain terms of pregnancy.
It can be determined by the doctor by the size of the uterus, which correspond to certain terms of pregnancy.
With sufficient certainty, it is possible to determine the duration of pregnancy and, therefore, childbirth according to the ultrasound examination of the fetus.
Birth before 37 weeks of gestation is considered premature, and after 42 weeks – late.
Term delivery, that is, on time, is considered a birth that began at full-term pregnancy. It is known that the duration of full-term pregnancy varies from 37 completed weeks (259days) up to 42 weeks (294 days). Starting at 38 weeks pregnant, you can expect to give birth every day.
Harbingers and onset of labor.
It is impossible to determine the date of delivery in advance, but there are a number of signs by which one can judge its approach.
Harbingers of childbirth:
1. The pregnant woman feels that she has become easier to breathe; this is due to the fact that the fetal head sank lower and pressed tightly against the entrance to the bone pelvis.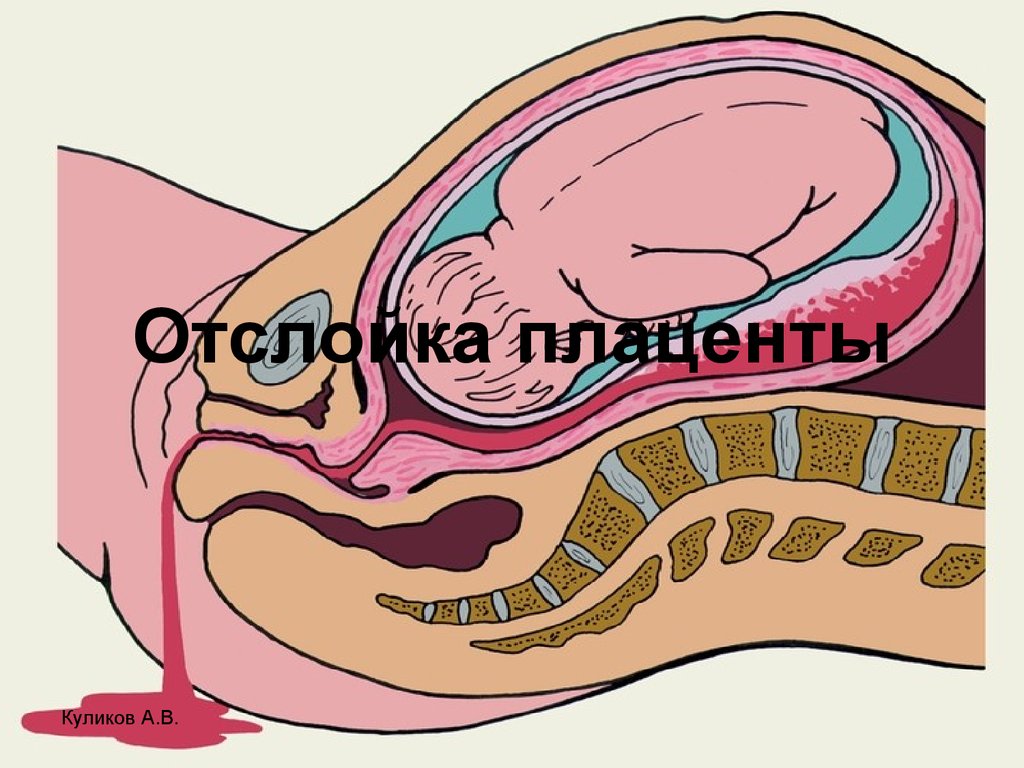 ;
;
2. The amount of vaginal discharge increases, it may turn brown or pink;
3. Separate uterine contractions appear – “training” contractions – irregular, short and quickly passing when stroking the abdomen;
4. In the lumbar region there are often weak, dull, quickly passing pains;
5. As a rule, a pregnant woman loses body weight.
When these warning signs appear, you should prepare for a trip to the maternity hospital. You can not go out of town and leave the house for a long time, as contractions may suddenly begin or amniotic fluid will pour out. But it is quite possible that you will have to be patient and wait. The interval between the appearance of precursors and childbirth can be several days, and 2-3 weeks.
Start of labor
The onset of labor is indicated by the appearance of bloody, spotting discharge from the vagina. This leaves the “birth plug”, that is, the contents of the cervix, which begins to open; the appearance of a “birth plug” means that labor will begin in the next 24-48 hours.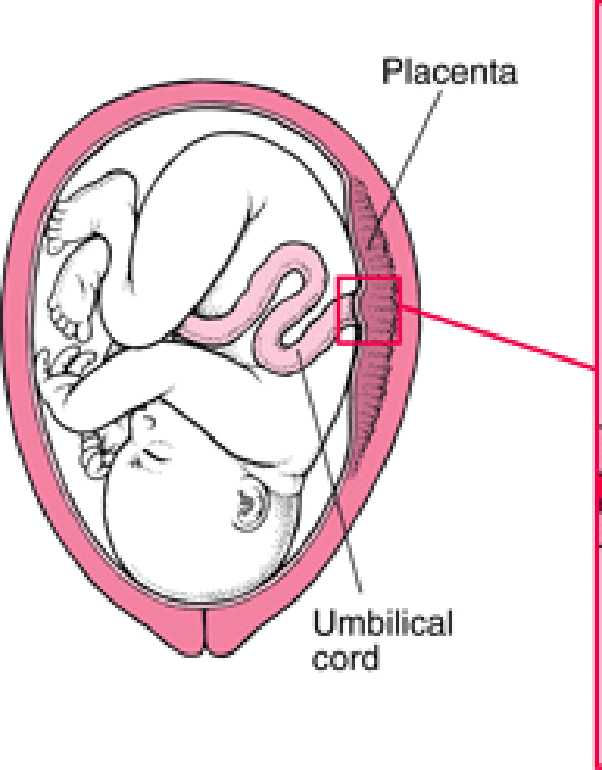
Amniotic fluid discharge
It is important to pay attention to the amount of water that can “gush” unexpectedly or pour out in a thin stream. Normally, the waters are light or slightly pinkish, without the admixture of bright blood, white lumps of the fetus’s original lubricant can be seen in them. However, the waters may have a greenish or brown color, which is due to the ingestion of the original feces – meconium. This should be reported to the doctor, as meconium in the waters may indicate fetal discomfort.
After the discharge of water, you must immediately go to the maternity hospital, as a long anhydrous period is fraught with the risk of infection of the fetus and the birth canal of the mother. To avoid infection, do not tightly close the vagina with a pad or insert a tampon, you can not take a bath, only a shower.
Regular labor pains
The main thing that is characteristic of labor pains is their regularity, repetition at first every 15-20 minutes, then more and more often, longer and stronger. These are true labor pains that open the cervix. In contrast, false contractions usually have an irregular rhythm, do not intensify and can stop if you change the position of the body. However, false contractions also perform an important function – they prepare the cervix for childbirth, which becomes soft, short, its channel opens, that is, it matures for childbirth.
These are true labor pains that open the cervix. In contrast, false contractions usually have an irregular rhythm, do not intensify and can stop if you change the position of the body. However, false contractions also perform an important function – they prepare the cervix for childbirth, which becomes soft, short, its channel opens, that is, it matures for childbirth.
Normal childbirth in nulliparous women lasts an average of 12-14 hours, and in multiparous women 6-8 hours.
Periods of childbirth
The onset of labor is considered to be the appearance of uterine contractions, rhythmically repeating every 10-15 minutes. Contractions gradually increase, and the interval between them decreases. With the onset of labor, a pregnant woman is already called a woman in labor.
If the delivery is too long, the woman is helped. Doctors of ancient Greece said that the sun should not rise twice over the head of a woman in labor.
There are three periods of childbirth: dilatation of the cervix, expulsion of the fetus and the postpartum period.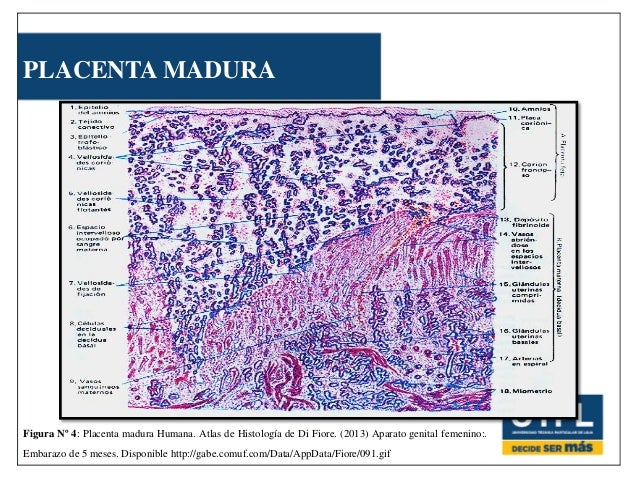
The first stage of labor is the gradual opening of the cervix
It occurs under the influence of regular contractions. Contractions over and over again stretch the circular muscles of the neck, making it thin and supple. The wedging of the fetal bladder into it and the pressure of the fetal head are also aimed at this. Slow, gradual opening of the cervix begins 2-3 weeks before delivery. In most women, the cervix “ripens” for childbirth, that is, it becomes short, soft, with a channel open by 2 cm.
The period of dilation is the longest in childbirth. It lasts about 9-10 hours for nulliparous women and 6-7 hours for multiparous women. The duration of contractions during this period increases to 1.5 minutes, and the interval between them decreases from 10-15 minutes to 1 minute.
In the first stage of labor, a woman in labor should follow the recommendations of the doctor and midwife and actively help herself: breathe calmly and evenly through the nose, relax outside the contraction. When the cervix opens completely, the fetal head can descend into the pelvic cavity.
The second stage of labor – expulsion of the fetus
When the head of the fetus reaches the exit of the pelvis, that is, sinks to its bottom, attempts are added to the contractions – contractions of the abdominal muscles. Due to this, intra-abdominal pressure increases, which helps to expel the fetus from the uterus.
The duration of the exile period is on average 1-2 hours in nulliparous women and less than an hour in multiparous women.
During the period of exile, it is especially important to follow the instructions of the doctor and midwife, helping yourself and the child to safely go through this very important stage. An experienced doctor and midwife will take the baby after birth, lightly pat him on the buttocks, the baby will scream, his lungs will expand, and he will begin to live an extrauterine life.
Childbirth is not yet completed – the child is still connected to the mother by the umbilical cord, and the placenta is in the uterine cavity. The afterbirth (children’s place) is the placenta, umbilical cord and membranes of the fetus.
In the third, consecutive period, the umbilical cord is cut
However, neither the mother nor the child will feel pain – there are no painful nerve fibers in the umbilical cord. The cry of a child immediately after birth is a good reaction to a new environment for him. A sign is put on the child’s pen, on which the surname, name and patronymic of the mother, the year, day and hour of birth of the child, as well as his gender are indicated.
The third stage of labor lasts on average 5-10 minutes, but can be delayed up to 1 hour. The woman in labor feels weak contractions that separate the placenta from the walls of the uterus, and then with one or two light attempts, the child’s place comes out. Now the birth is over.
After giving birth, a woman (she is now called not a woman in labor, but a puerperal) stays in the maternity ward for two hours under the close supervision of medical personnel who monitor the condition of the woman and the amount of bloody discharge from the genital tract. At this time, the soft birth canal is examined and, if there are gaps, then sutures are applied with preliminary anesthesia. After the examination, the puerperal is transferred to the postpartum department.
At this time, the soft birth canal is examined and, if there are gaps, then sutures are applied with preliminary anesthesia. After the examination, the puerperal is transferred to the postpartum department.
How to make childbirth easier
Childbirth is a hard physical strain. A pregnant woman needs to learn how to use her energy sparingly. Fear of labor pain interferes with the proper course of childbirth. To learn how to manage labor pain, a pregnant woman must master some techniques.
First of all, it concerns the posture during childbirth. At the beginning of labor, when the contractions are still irregular and short, you can choose the position of the body that will be most convenient. However, lying on your back is not recommended, because in this position the fetal head compresses the mother’s large blood vessels, reducing blood flow to the placenta.
A simple and important rule is to urinate frequently. It is necessary to urinate every two hours, as a full bladder prevents the fetal head from descending into the pelvic cavity.
In the active stage of labor, when contractions are frequent, it is also necessary to regularly change the position of the body, trying not to lie on your back. If doctors allow you to walk, this should be used. You can kneel in bed, leaning on a chair, that is, tends to change the position of the body more often.
Recently, some maternity hospitals recommend that the first stage of labor be carried out in a warm water bath. Immersion in warm water relieves painful contractions and has a calming effect on the woman in labor. However, the second stage of labor must be carried out traditionally. When the expulsion of the fetus begins, the attempts are delayed, it is possible, if the doctor allows, to squat down during the fight, since in this position the dimensions of the pelvis increase and the head of the fetus falls more easily. Between contractions, it is better to lie on your side or take a knee-elbow position. When attempts appear and the birth of the fetus begins, the woman in labor is transferred to another ward, to a special bed designed for childbirth.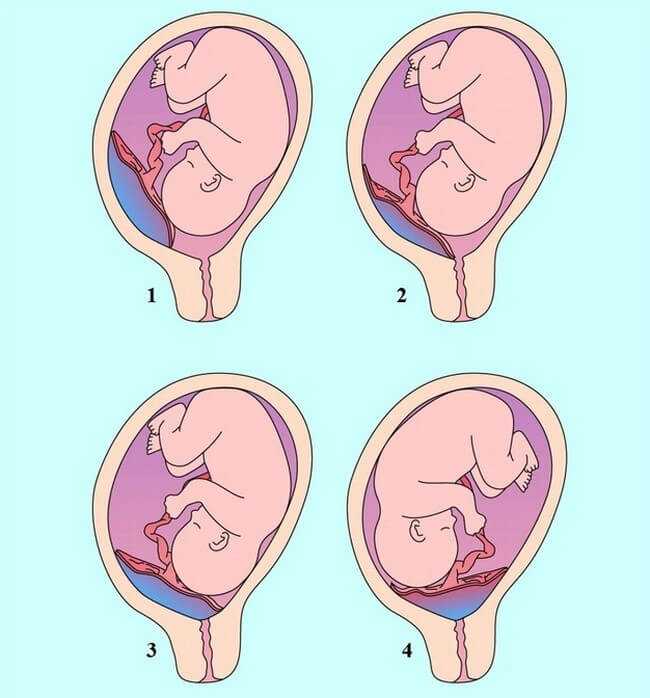 Here, usually the medical staff manages the position of the mother, facilitating childbirth.
Here, usually the medical staff manages the position of the mother, facilitating childbirth.
It is very important for a woman to learn how to breathe properly during contractions and to relax completely between them. During contraction, due to muscle contraction, the fetus receives less oxygen. Therefore, its lack in these moments must be compensated by proper breathing.
In the first stage of labor, when contractions are repeated after 8-10 minutes and last for 40-50 seconds, it is necessary to use the first type of breathing – slow and deep.
Childbirth is less painful and more gentle for the fetus, when the woman in labor alternately walks, then lies on her side, that is, the active position alternates with the resting position.
When contractions become more intense, recur after 5-6 minutes and last about one minute, it is recommended to use shallow breathing (second type). With the beginning of the fight, it is better to make several deep, slow breaths according to the first type, and with the increase in the fight, you need to switch to shallow breathing, but then, at the end of it, switch back to slow and deep breathing.
At the end of the first stage of labor, when contractions are stronger, repeat after 2-3 minutes and last for 60-90 seconds, shallow and fast breathing should be applied. It is like a dog breathing with its mouth open on a hot day. So you need to breathe only at the height of the fight. With the beginning of the fight, you can apply the first, and then move on to the second and third types of breathing.
When pushing, it is also useful to use the third type of breathing, taking small intervals to inhale air. At this time, do not strain the abdominal muscles. At the same time, the head of the fetus is not squeezed out by attempts, but, as it were, is pushed by exhalations, and the child is born easier.
It is best to remain relaxed during the contraction. But this relaxation is not passive, but active – a conscious process that requires concentrated attention. Here, the woman in labor should use the relaxation techniques that she mastered during pregnancy. During this period, the self-hypnosis formula is applied: “I am calm. Contraction is an indicator of labor activity. Gradually, the contractions will intensify. My breathing is even and deep. The muscles are relaxed. The fight is over, after that there will be a rest period.
Contraction is an indicator of labor activity. Gradually, the contractions will intensify. My breathing is even and deep. The muscles are relaxed. The fight is over, after that there will be a rest period.
There is an idea that childbirth is necessarily accompanied by pain. It is the rooted fear and expectation of pain that become, especially in impressionable, nervous women, factors that intensify unpleasant sensations and raise them to the degree of pain.
Obstetricians are well aware that the normal course of childbirth is not necessarily accompanied by pain. In about 20% of women, childbirth is accompanied by only minor pain. Moreover, women of some nationalities do not know at all what pain during childbirth is.
Don’t be afraid of pain! Even if it occurs, the doctor will be able to alleviate it, modern obstetrics has great opportunities for this.
Widespread use in clinical practice has found a variety of painkillers, used in doses that are absolutely harmless to the mother and fetus.