La placenta es un órgano vital para el bebé en formación, ya que le proporciona oxígeno y alimento y se encarga de eliminar los desechos del feto. Habitualmente, la placenta está localizada en la zona alta o lateral del útero; pero en ocasiones se inserta en otros lugares. Hablamos entonces de placenta previa o de placenta de inserción baja.
¿Qué implicaciones tiene para el curso del embarazo? ¿Es peligroso para el bebé? ¿Cómo determina el tipo de parto?
No te lo pierdas:
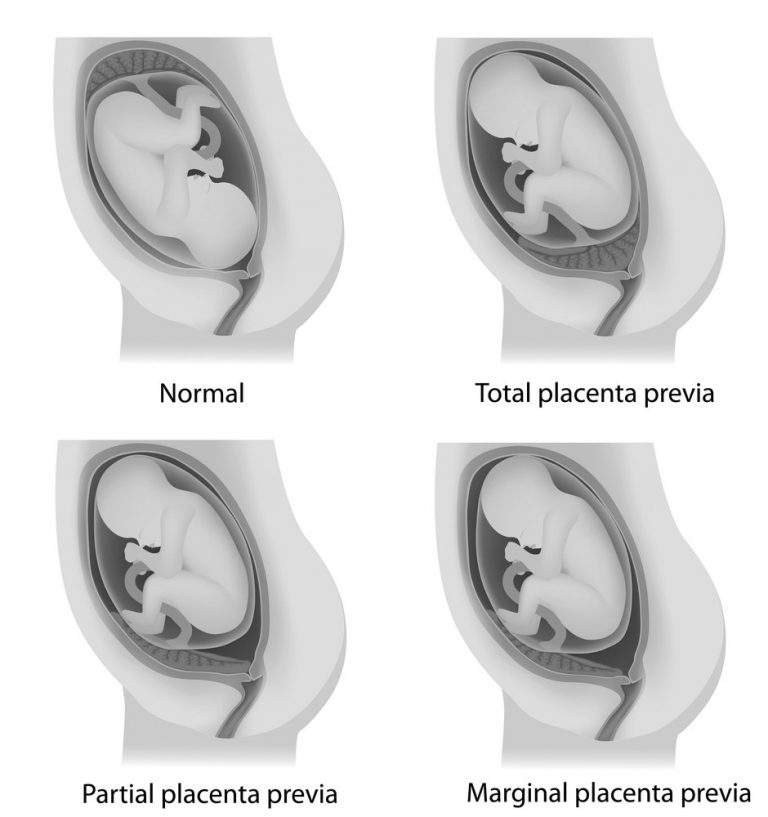
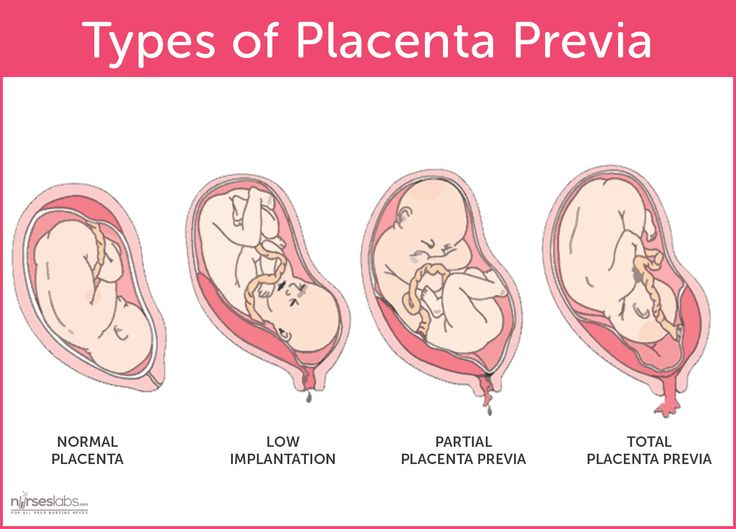
La placenta previa puede ser oclusiva total, oclusiva parcial o marginal. La primera es la que tapa completamente el canal del parto, el cuello el útero, “por lo que, si se mantiene así, el niño no puede nacer por vía vaginal”, explica la Dra. Yoana Chiverto, ginecóloga adjunta del Hospital Universitario Sanitas La Moraleja, de Madrid y miembro de la Unidad de Alto Riesgo Obstétrico del citado centro.
En cuanto a la placenta previa oclusiva parcial, es aquella que no ocupa todo el canal del parto, aunque también implica una cesárea por el alto riesgo de sangrado. Hablamos de placenta previa marginal cuando se sitúa en el lateral del cuello del útero, pero sin llegar a cubrirlo.
Por otra parte, hay que diferenciar entre placenta previa y placenta baja (o de inserción baja). La placenta baja puede situarse a una distancia variable del cuello del útero (dos centímetros, un centímetro…), pero “lo habitual es que al ir creciendo el útero, la placenta se vaya desplazando a su lugar”, indica la especialista. Así, el parto no estaría condicionado finalmente por la situación de la placenta.
En la mayoría de los casos, la placenta previa es asintomática, por lo que la embarazada no reconoce el problema. La forma de saber la inserción de la placenta es mediante ecografía.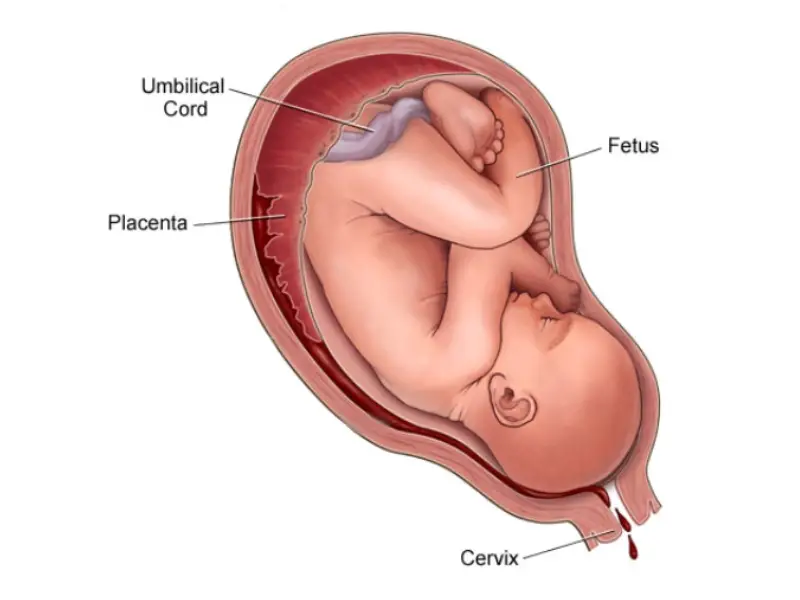 Así, en la eco de las 20 semanas, una prueba que arroja muchos datos trascendentales, se determina dónde está insertada la placenta.
Así, en la eco de las 20 semanas, una prueba que arroja muchos datos trascendentales, se determina dónde está insertada la placenta.
Posteriormente, en el tercer trimestre del embarazo, entre la semana 32 y la semana 34, se vuelve a hacer otra ecografía donde se confirmará el lugar en el que está situada y si finalmente hay contraindicaciones para el parto vaginal.
©AdobeStock
“Cuando la placenta previa se diagnostica en la semana 20, hay que hacer un control más exhaustivo a la mujer para ver si se desplaza a normal o se queda en placenta previa”, explica la Dra. Chiverto.
Además, la embarazada debe seguir estas pautas:
No se saben los motivos por los cuales la placenta, en lugar de insertarse en el lugar que le corresponde, se adhiere a otro lugar. No obstante, hay algunos factores que predisponen a la placenta previa. Son los siguientes, según detalla la especialista del Hospital Universitario Sanitas La Moraleja:
Aunque se diagnostique una placenta previa en la semana 20 de embarazo, afortunadamente, la gran mayoría de las placentas acaban insertándose bien, según avanza la gestación, de modo que, tal como apunta la Dra.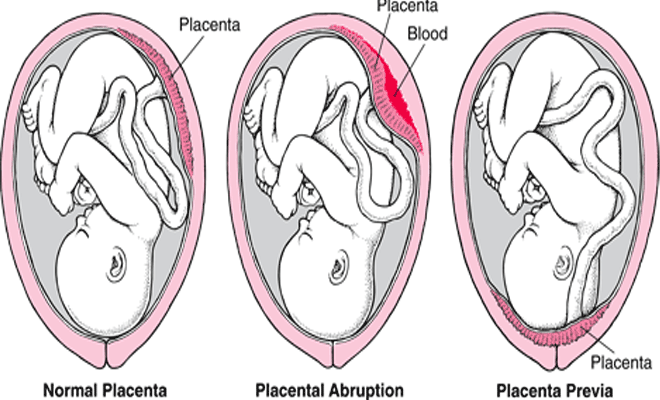 Yoana Chiverto, “al final del embarazo tan solo hay un 0,25-0,5% de placentas previas reales”.
Yoana Chiverto, “al final del embarazo tan solo hay un 0,25-0,5% de placentas previas reales”.
Si el diagnóstico se ha mantenido hasta el final de los nueve meses, habrá que hacer una cesárea obligatoriamente. Pero si la placenta ya se ha colocado en su lugar correcto, el parto puede ser por cesárea o vaginal, dependiendo de las circunstancias concretas.
La placenta previa no supone ningún peligro para el feto durante el embarazo, ya que cumple sus funciones a la perfección. Pero en gestaciones no controladas en las que se llega al final sin diagnóstico de placenta previa, las contracciones pueden desencadenar sangrados importantes con riesgo vital para la madre y el bebé. Si hay un control y un diagnóstico previos, no habrá problema, pues se programará una cesárea para no correr riesgos innecesarios.
No te lo pierdas
© ¡HOLA! Prohibida la reproducción total o parcial de este reportaje y sus fotografías, aun citando su procedencia.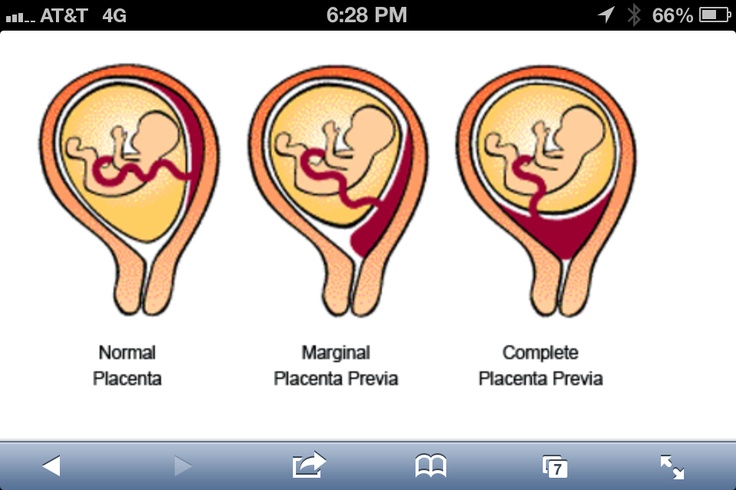
La placenta previa se diagnostica mediante una ecografía, ya sea durante una cita médica prenatal de rutina o después de un episodio de sangrado vaginal. La mayoría de los casos de placenta previa se diagnostican durante una ecografía en el segundo trimestre.
El diagnóstico inicial puede hacerse con un dispositivo de ecografía sobre el abdomen. Es posible que para obtener imágenes más precisas necesites una ecografía transvaginal, en la que se utiliza un dispositivo con forma de varilla que se coloca dentro de la vagina. El proveedor de atención médica tendrá cuidado con la posición del dispositivo para no romper la placenta ni causar sangrado.
Si te diagnostican placenta previa durante un examen de rutina, es probable que debas realizarte ecografías más frecuentes para controlar los cambios en la placenta.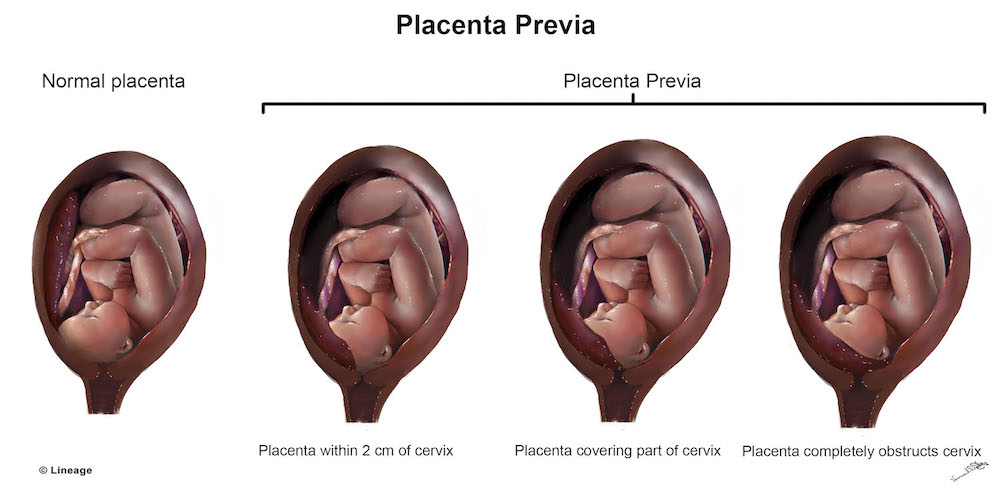
En muchas mujeres a las que se les diagnostica placenta previa al comienzo del embarazo, la afección se resuelve por sí sola. A medida que el útero crece, es posible que aumente la distancia entre el cuello del útero y la placenta. Además, es posible que la placenta crezca en dirección a la parte superior del útero, y que los bordes de los tejidos placentarios cerca del cuello del útero se encojan.
Si la placenta previa se resuelve, es posible que puedas planificar un parto vaginal. Si no se resuelve, deberás planificar un parto por cesárea.
El sangrado vaginal de más de 20 semanas se trata como una emergencia médica. Podrías ingresar a la unidad para el trabajo de parto y parto. Tú y tu bebé estarán bajo supervisión y es posible que necesites una transfusión de sangre para reemplazar la sangre perdida.
Si llevas 36 semanas de embarazo, es probable que te hagan una cesárea para que nazca el bebé. Si has perdido mucha sangre o si existe un riesgo de salud para ti o el bebé, es posible que necesites una cesárea de emergencia antes de las 36 semanas.
Si es la primera vez que has tenido un sangrado y este se detuvo durante al menos 48 horas, es posible que te den el alta hospitalaria. Si continúas teniendo sangrados más intensos, el equipo de atención médica podría recomendar que permanezcas en el hospital.
Cuando no hay sangrado, el objetivo del tratamiento es reducir los riesgos de que este se desarrolle y de acercarte a tu fecha de parto tanto como sea posible. Es probable que tu proveedor de atención médica te recomiende evitar lo siguiente:
Si te dan de alta del hospital después de un primer episodio de sangrado, deberás seguir estas recomendaciones para reducir el riesgo de tener un segundo episodio.
Te aconsejarán que busques atención médica de emergencia si tienes sangrado vaginal o contracciones.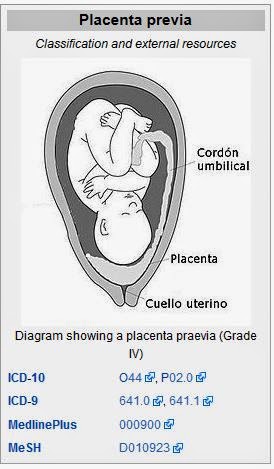 Tu proveedor de atención médica podría preguntarte si alguien te ayudará en casa y si te pueden llevar a un hospital cercano.
Tu proveedor de atención médica podría preguntarte si alguien te ayudará en casa y si te pueden llevar a un hospital cercano.
Aunque no hayas presentado sangrado durante el embarazo debido a la placenta previa (o no hayas tenido ningún sangrado desde el primer episodio) es probable que se programe un parto por cesárea entre las 36 y las 37 semanas.
Si el parto está planeado para antes de las 37 semanas, tu proveedor de atención médica te dará corticoides para ayudar a desarrollar los pulmones del bebé.
Solicite una Consulta en Mayo Clinic
Si te diagnostican placenta previa, posiblemente te preocupe cómo esta afección afectará a tu bebé, a tu familia y a ti. Algunas de estas estrategias pueden ser útiles para enfrentar la situación:

La placenta previa se suele diagnosticar durante una ecografía de rutina o después de un episodio de sangrado vaginal. Por lo tanto, es posible que no tengas tiempo de prepararte para una cita médica de placenta previa como lo harías para las típicas citas de atención prenatal.
Si no necesitas atención médica inmediata o te envían a casa después de un tratamiento por sangrado vaginal, es importante que entiendas el plan de control y atención médica continua.
Estas son algunas de las preguntas que podrías hacerle a tu proveedor de atención médica después de un diagnóstico o en los exámenes de seguimiento:
Es probable que tu proveedor de atención médica te haga diversas preguntas sobre tu capacidad de gestionar la atención médica en el hogar, especialmente si ya tuviste un episodio de sangrado. Estas son algunas preguntas de ejemplo:
Estas son algunas preguntas de ejemplo:
Escrito por el personal de Mayo Clinic
19th week
21 weeks
20 weeks is a significant period, because half the journey has already been completed. And if there are no complications and complaints, you can feel the happiest. But even if there are complications, you should not concentrate on them and worry. After all, the nervous system is now also very important. Doctors have long known everything about every stage of pregnancy and have learned to help expectant mothers with any specific cases.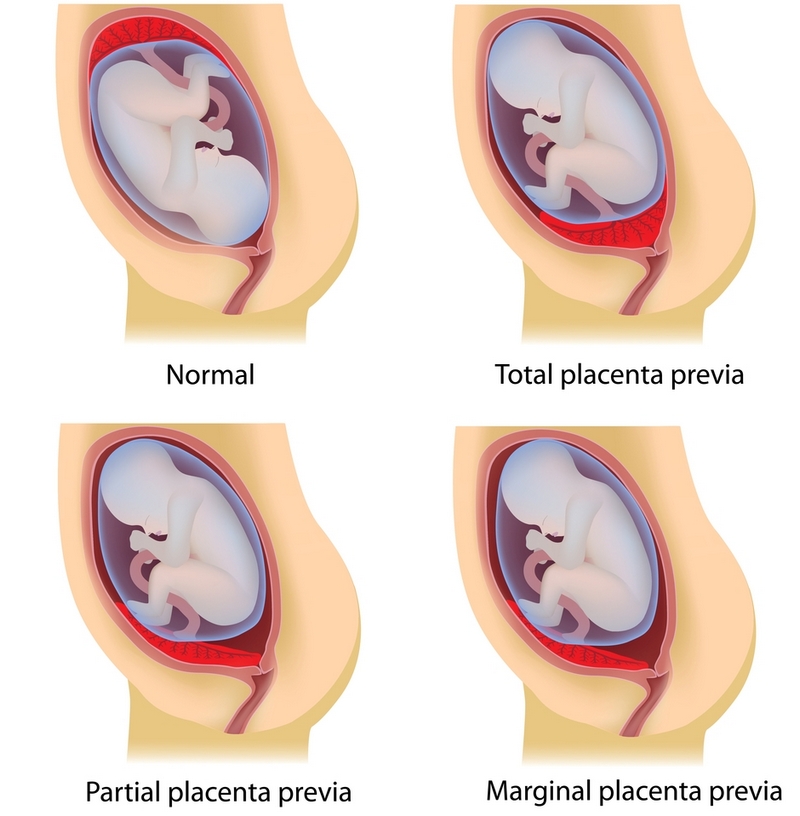 You need to find a doctor you can trust. We hope that you have such a doctor.
You need to find a doctor you can trust. We hope that you have such a doctor.
On the 20th week, the internal organs of the little man, as well as his endocrine system, have formed and perform the functions assigned to them. There are already convolutions in the child’s brain, and the parts of the brain themselves are improving every day. If earlier it was about imitation of sucking movements, now the fetus can really swallow. Its subcutaneous fat layer increases. A blink reflex appears, facial expressions are expressed. If you do an ultrasound, then from this period the volumes of the fetus are already measured – the diameter of the head (approximately 46.6 mm), chest (46.4 mm), abdomen (47 mm). The thickness of the placenta is also measured: at this time it is about 22 mm. There is placenta previa. This means that the placenta is located so low that it overlaps the cervix. But the uterus is still growing for half the term, and during this time the placenta usually rises along with the growing uterus.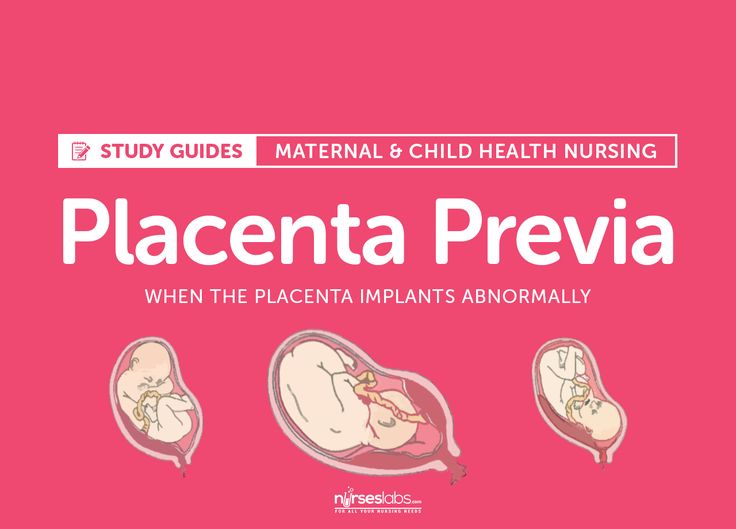 If the growth of the uterus does not affect the change in the situation, then delivery by caesarean section will be done. With strong fetal pressure on the placenta previa, spotting occurs. This condition requires hospitalization and urgent treatment.
If the growth of the uterus does not affect the change in the situation, then delivery by caesarean section will be done. With strong fetal pressure on the placenta previa, spotting occurs. This condition requires hospitalization and urgent treatment.
At this time, all women feel movements. Even close hands can feel the movement of the fetus. He lives your life more and more: when loud sounds and other negative stimuli appear, or if the mother is in a stuffy room, the fetus reacts with active actions. And vice versa: with the sounds of calm music, with a good mood of the mother, while walking in the fresh air, the movements of the baby are calmer. Women are advised to count how many times in an hour she feels a stir. Ideally, there should be one stir every ten minutes during his active period. And do not be upset if the baby does not make itself felt for some time – this means that he is sleeping. The height of the fundus of the uterus during this period is approximately 18-20 cm (navel area). The tummy is rounded so much that the waist has disappeared. The lower back may ache. In this case, with the help of a doctor, pick up a bandage and wear it for long walks. It is also recommended to do simple exercises for the spine and wear shoes with arch supports and flats.
The tummy is rounded so much that the waist has disappeared. The lower back may ache. In this case, with the help of a doctor, pick up a bandage and wear it for long walks. It is also recommended to do simple exercises for the spine and wear shoes with arch supports and flats.
One of the consequences of pregnancy in the absence of gymnastics is lordosis, which is characterized by an increased deflection in the lumbar region. A dark line appears on the midline of the abdomen, and the first stretch marks appear on the sides. To avoid stretch marks on the chest, which is still not always possible, you should choose a comfortable bra made of natural materials with wide straps. If there are marks on the skin from jewelry or clothes, you need to adjust the diet and check the kidneys with your doctor. This may be a sign of puffiness. Vaginal discharge during pregnancy should be mucous, a little thicker than usual. If purulent, flaky discharge appears, it is necessary to take a smear for analysis. Bloody discharge can be both with placenta previa and with the threat of miscarriage. Therefore, an urgent appeal to specialists and hospitalization is necessary at the first appearance of spotting.
Bloody discharge can be both with placenta previa and with the threat of miscarriage. Therefore, an urgent appeal to specialists and hospitalization is necessary at the first appearance of spotting.
What is breech and cephalic presentation of the fetus and can the position of the fetus be influenced? Dikan gymnastics. Why is chorion previa or placenta previa dangerous? Doctors of medical clinics “Art-Med” answer questions about the presentation of the fetus and placenta.
Ask a Question
Pregnancy 19 weeks – breech presentation, what to do?
Nothing. At this time, the baby in the uterine cavity is actively moving in any direction. After 5 minutes he was already in a different position.
At 32 weeks I was diagnosed with marginal placenta previa, there is no tone, the cervix is high, I have been lying on the preservation for 3 weeks.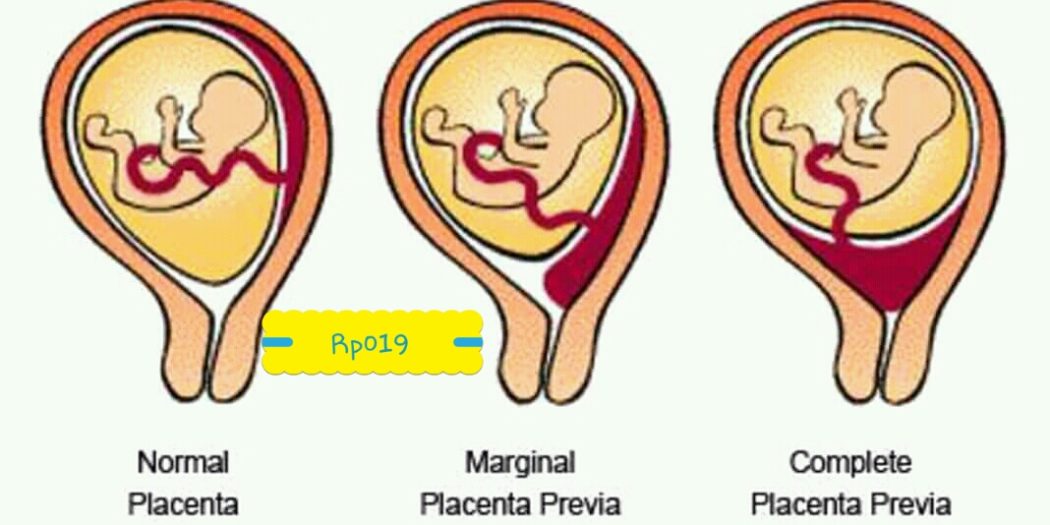 What are my prospects, will I be able to carry the pregnancy?
What are my prospects, will I be able to carry the pregnancy?
How long a pregnancy can be carried depends on many factors. It is necessary to follow the recommendations of doctors, adequate therapy and a great desire to give birth to a healthy baby on time.
Pregnancy 33 weeks, low placentation was delivered (the placenta is located on the anterior wall of the uterus, the thickness of the placenta is 44 mm, the placenta recedes from the internal os – 48 mm, the structure of the placenta is heterogeneous, calcifications along the periphery, the degree of maturity is 2, which corresponds to the gestational age ). What does this mean and what could be the consequences?
The placenta is located normally. Thickening of the placenta can be observed both in normal conditions and with intrauterine infection, immunological disorders, and so on. An examination is needed to clarify the situation. You are at increased risk of developing placental insufficiency.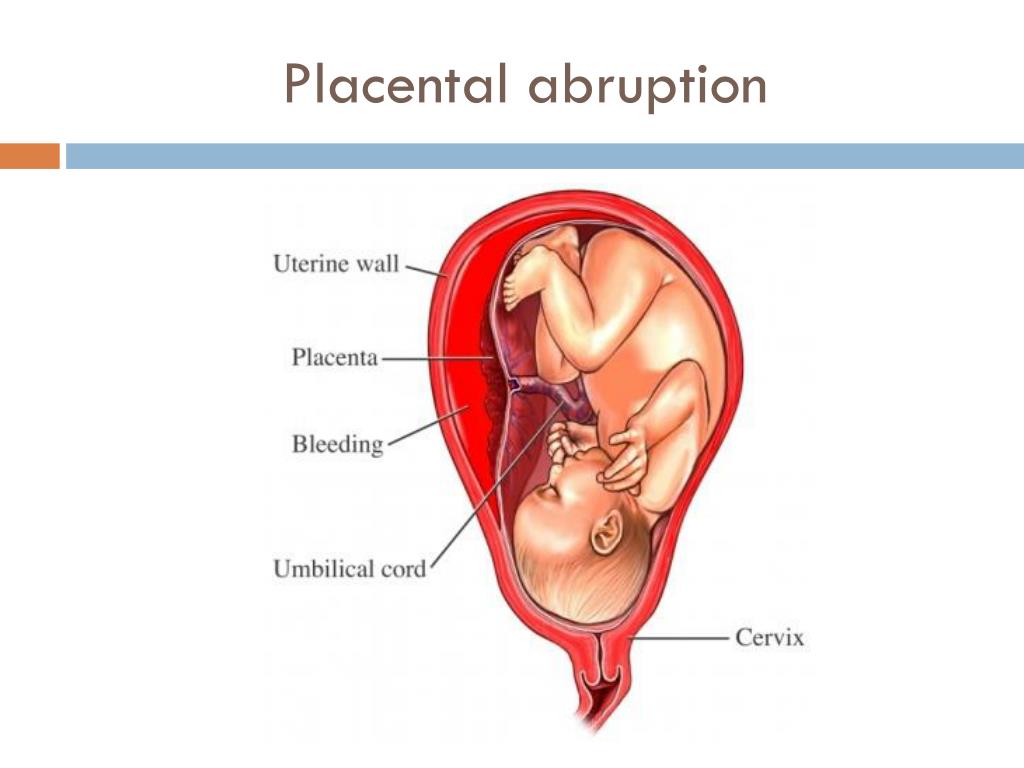
From the age of 4 months I started to have edema, my blood pressure is 110/70, sometimes it rises to 120/80 and 130/90, in January at 30 weeks I went to the hospital, an ultrasound showed a thickening of the placenta. Exactly a month passed and I was again hospitalized with high blood pressure, an ultrasound showed swelling of the placenta. How does placentitis affect a child, is it worth doing a premature birth at 37-38 weeks and what method of delivery is used in this situation?
Thickening of the placenta can be observed not only with placentitis. While the placenta copes with its work (the baby grows up according to the deadline), its changes are not dangerous. If your pressure is not normalized, or the baby suffers, an early delivery will be required. In what way – depends on the specific situation.
I am 23 years old, second pregnancy, 24 weeks. Ultrasound revealed placental hyperplasia with cystic changes, partial placenta previa along the posterior wall, degree of maturity 1-2.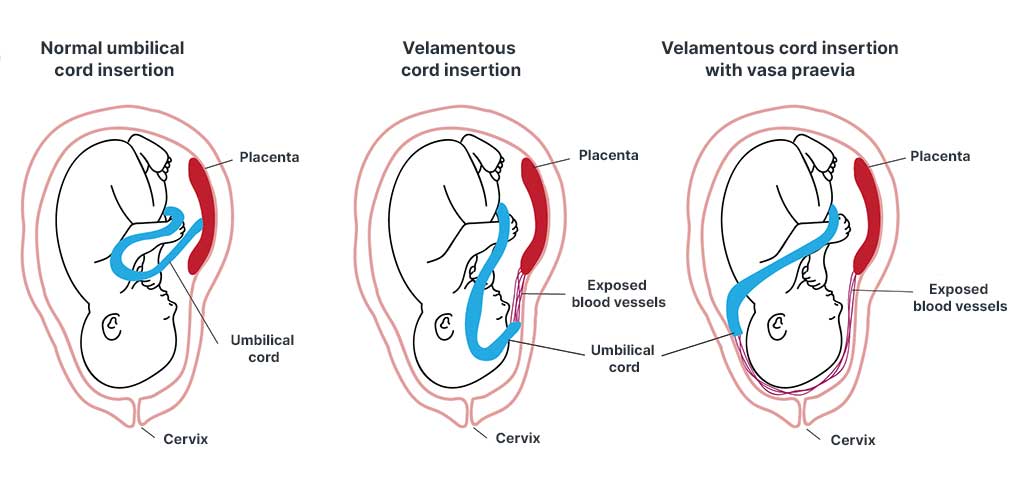 The strange thing is that 2 weeks before that, an ultrasound was also done in the hospital and everything was in order with the placenta. In the interval between ultrasounds, she had an acute respiratory viral infection with a strong cough, could this have had such an effect on the deterioration of her condition? Is there a chance that after a complete cure for a cold, the placenta will return to its previous state?
The strange thing is that 2 weeks before that, an ultrasound was also done in the hospital and everything was in order with the placenta. In the interval between ultrasounds, she had an acute respiratory viral infection with a strong cough, could this have had such an effect on the deterioration of her condition? Is there a chance that after a complete cure for a cold, the placenta will return to its previous state?
Viral infection may have caused changes in the placenta. The infection has nothing to do with placenta previa. To clarify the situation, I recommend repeating the ultrasound in 2-3 weeks.
My gestational age is 24 weeks, low placentation on the posterior wall of the uterus, uterine hypertonicity, the internal os reaches but does not overlap, the internal os is closed, is it possible for the placenta to migrate, will a bandage help with this, what medications can be taken to tone the uterus back to normal?
The placenta may still rise. But treatment is not prescribed in absentia. Come to the reception.
But treatment is not prescribed in absentia. Come to the reception.
I am 40 weeks pregnant. On ultrasound at 35 weeks, head diligence was written, but I feel tremors in the lower abdomen near the pubic bone. Could the doctor make a mistake during the ultrasound and I have a breech presentation?
To clarify the situation, either an examination or repeated ultrasound diagnosis is necessary. The baby could roll over.
At 29 weeks my gynecologist said the baby was in a breech presentation. Ultrasound at 30 weeks showed a headache, today the gynecologist again put the pelvic, term-34 weeks. Will the fetus turn over correctly before the end of the term?
Until 36 weeks, the baby can still turn. With polyhydramnios, the fetus can “spin” even during childbirth.
At 13.4 weeks of pregnancy, I have an ultrasound report: low placentation, predominant localization of the chorion: posterior at the level of the internal os.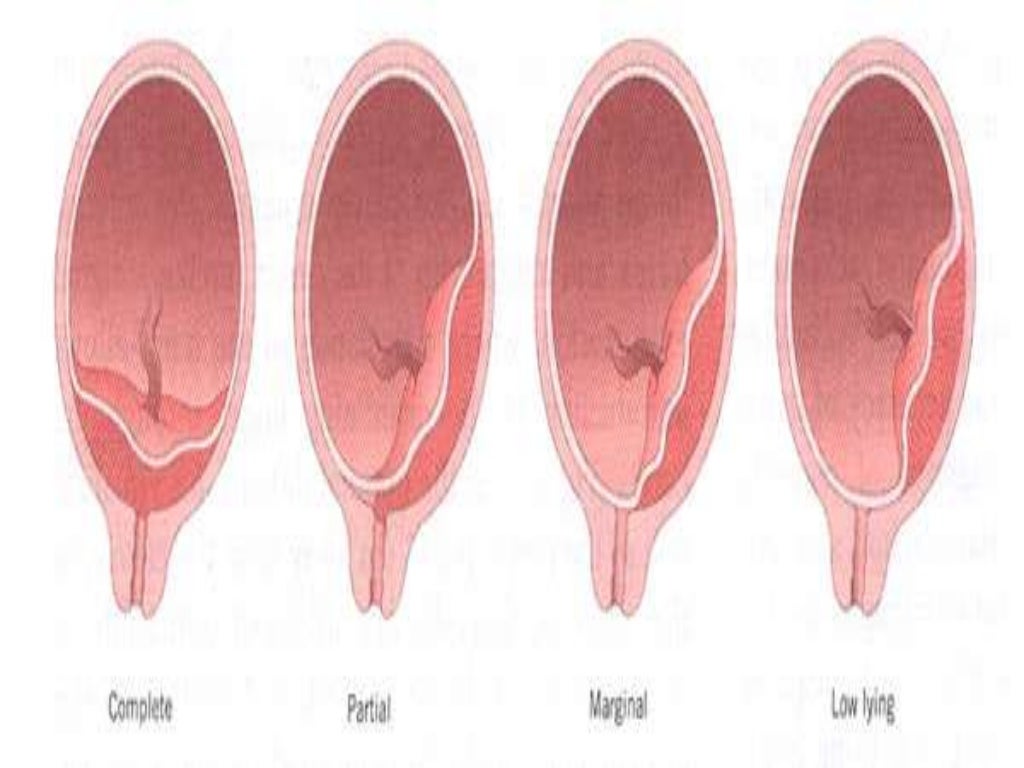 Is it possible to go to the pool or do you need complete rest?
Is it possible to go to the pool or do you need complete rest?
You can go to the pool, but it is undesirable to have sex and run and jump.
At the gestational age of 15 weeks and 3 days, according to ultrasound, a marginal placenta previa along the anterior wall of the uterus on the right reaches and overlaps the internal os. Can the placenta “rise”, if so, when?
Yes, maybe closer to 20 weeks pregnant.
At 15 weeks and 3 days of pregnancy, she was diagnosed with low placentation. Is it dangerous and how can it affect the development of the fetus?
At this time, the low location of the placenta is a variant of the norm. With the growth of the uterus, the placenta should “rise”. If this does not happen, the situation will be considered as placenta previa with all the ensuing consequences. Read more about this in the Medical Publications section.
Pregnancy 35 weeks, at 32 weeks she did an ultrasound, the placenta is 5 cm higher than the internal os, along the anterior wall of the uterus. Can it rise to 38 weeks, is it necessary to do a second ultrasound and for how long?
Can it rise to 38 weeks, is it necessary to do a second ultrasound and for how long?
The placenta is located normally. Repeat ultrasound at 37 weeks gestation.
Ultrasound revealed that I have placental hyperplasia, increased to 46 mm, period 32 weeks 2 days. Why is this happening, how dangerous is it? With placental hyperplasia, childbirth takes place usually or by caesarean section?
Thickening of the placenta can be observed both in the norm (with its small area), and with intrauterine infection, fetal malformations, immunological problems, etc. An examination is necessary to clarify the situation. The thickness of the placenta does not affect the method of delivery.
I have a bicornuate uterus, incomplete septum, 12.5 weeks pregnant. She was in the hospital from 6 to 9 weeks with the threat of interruption. There were about 4 ultrasounds (the first at 5 weeks) that diagnosed pregnancy in the left horn. Now the CTE is 65 mm, the organs are being visualized, the chorion is 13 mm. The diagnosis is “complete placenta previa”. I don’t have any complaints. This can be if the pregnancy was in the left horn? As I understand it, the chorion cannot migrate down?
Now the CTE is 65 mm, the organs are being visualized, the chorion is 13 mm. The diagnosis is “complete placenta previa”. I don’t have any complaints. This can be if the pregnancy was in the left horn? As I understand it, the chorion cannot migrate down?
Placenta previa may well be in this situation – apparently, there was nowhere for it to “attach” above.
Diagnosed at 18 weeks. The lower edge of the placenta: from the lower edge, the amniotic cord is determined to the additional lobe, which is located along the posterior wall of the uterus (size 52 * 15 mm), the amniotic cord covers the internal os. And previa of the accessory lobe of the placenta. How dangerous is it?
Placenta previa, even its accessory lobe, is a serious complication of pregnancy. Read more about this in the Medical Publications section. The amniotic cord may not interfere with the course of pregnancy, but may cause malformations of the limbs and other parts of the fetal body, and may also be observed with chromosomal abnormalities. You need to go see a geneticist.
You need to go see a geneticist.
At 22 weeks of gestation, ultrasound showed complete placenta previa and cervical shortening up to 20 mm. In my case, can I put a pessary? And are there any chances for its lengthening with bed rest and placenta elevation?
Both suturing and insertion of a pessary in placenta previa is dangerous. There remains hope for bed rest and drug treatment aimed at normalizing the tone of the uterus.
This is my second pregnancy, 35-36 weeks, breech presentation. The plug started to come off. All indicators are normal. Will I be able to give birth at this time myself with a breech presentation? Isn’t it too early for the cork to come off? What should my gynecologist tell or find out during the examination?
If labor activity is good, you will be able to give birth yourself. The cork can also come off a month before the birth. The doctor should clarify the size of the fetus, your pelvis, the condition of the cervix.
I have placenta previa. Pregnancy 17 weeks. Doctors categorically forbid swimming in the sea. Why?
Swimming in the sea is not contraindicated for you. But long journeys and flights – yes.
My due date is 24 weeks. On ultrasound they wrote head diligence. But I feel tremors in the lower abdomen near the pubic bone. Could this be the case, or could the ultrasound be wrong?
At this time, the baby constantly turns around, at the time of the study, he may have been head down, and after 5 minutes he could turn his butt down. This is fine.
Can the doctor tell the approximate weight of the child by the size of the fundus of the uterus and the circumference of the abdomen?
The estimated fetal weight (in grams) can be calculated by multiplying the abdominal circumference (in cm) by the fundal height (in cm).
Pregnancy 12 weeks, twins.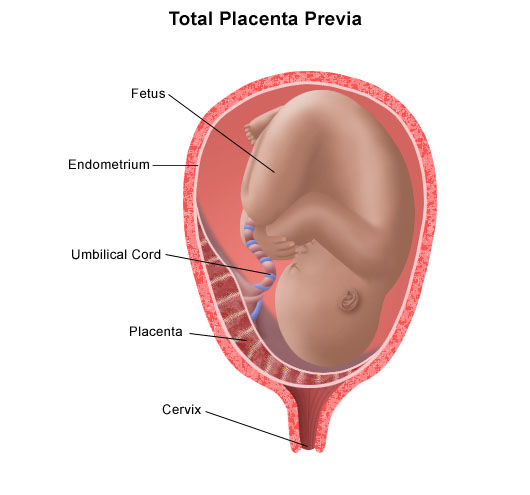 The placenta on the back wall, with the transition to the front, covers the internal pharynx. Can the placenta migrate? I don’t work, I lie a lot. What is the likelihood of complications, and in case of bleeding, will I be able to get to the hospital in time?
The placenta on the back wall, with the transition to the front, covers the internal pharynx. Can the placenta migrate? I don’t work, I lie a lot. What is the likelihood of complications, and in case of bleeding, will I be able to get to the hospital in time?
In multiple pregnancies, the placenta(s) occupy a large area of the uterus, so migration from the internal os is often difficult. So far, there is no cause for concern. If after 20 weeks of pregnancy the placenta does not rise, and bloody discharge from the genital tract appears, treatment in a hospital will be required. Obstetric bleeding is unpredictable in terms of its rate and volume of blood loss.
I am 28 weeks pregnant and diagnosed with placenta previa. I work physically, but I heard that it is dangerous. What should I do to avoid possible bleeding and any other complications? Should I leave work and stick to bed rest? I also heard about the migration of the placenta, can something change at this time?
You need to avoid physical activity, especially since it shouldn’t be a problem at work – pregnant women are required to be transferred to light work by law.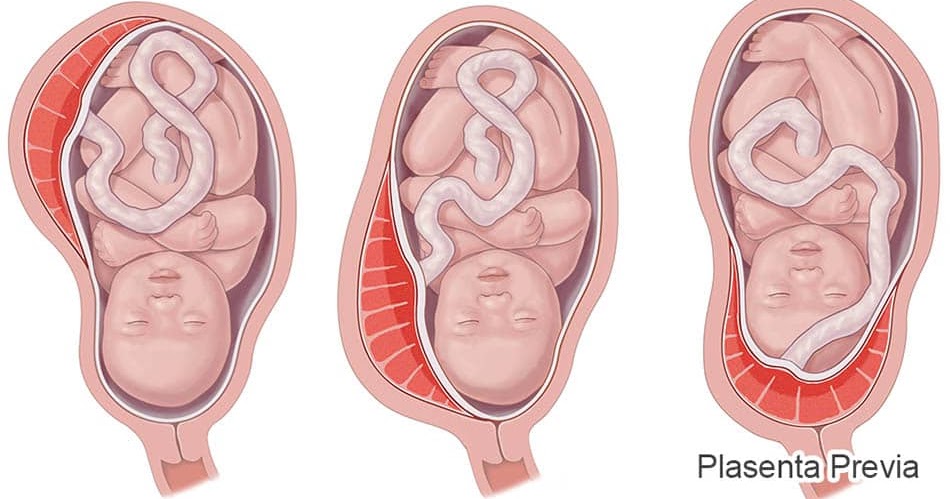 Migration of the placenta, of course, is possible, but at this time it is already unlikely. If placenta previa persists until childbirth, then a caesarean section will need to be done.
Migration of the placenta, of course, is possible, but at this time it is already unlikely. If placenta previa persists until childbirth, then a caesarean section will need to be done.
Ultrasound showed CTE 56 mm and determined the period of 12 weeks 5 days. The placenta is on the back wall and covers the internal os by 15 mm. How to understand this proposal correctly and what measures to take to prevent unpleasant consequences?
Your fertilized egg is attached low, mainly along the back wall, but part of the placenta is still blocking the exit from the uterus (internal os). That is, we are talking about placenta previa. Read more about this pathology in the publications section.
Ultrasound (16 weeks) revealed low placenta previa, uterine tone increased. Hospitalization was not offered. Is there a possibility that the state of the placenta may still change?
Yes, the placenta will most likely rise. This can be tracked at the next ultrasound (at 20-24 weeks of pregnancy). If you do not have spotting and threatened miscarriage, you do not need hospitalization now. However, you should avoid significant physical exertion (more than your usual) and constipation, as well as refuse sex.
This can be tracked at the next ultrasound (at 20-24 weeks of pregnancy). If you do not have spotting and threatened miscarriage, you do not need hospitalization now. However, you should avoid significant physical exertion (more than your usual) and constipation, as well as refuse sex.
I am pregnant after IVF 13 weeks, severe form of hyperstimulation with ovarian sizes 132 and 94 with many functional cysts, symmetrical placenta previa. The fetus is currently developing without pathologies. What is the likely prognosis for the development of pregnancy, is it possible for me to hope for a favorable outcome? Do you have specialists so that I can contact you for expert advice?
Since your pregnancy is desired, you must keep it. Most likely, you will have to spend most of it in the hospital. You have an increased risk of spontaneous abortion, bleeding, preeclampsia and other complications. But with proper management, you may well endure and give birth to a healthy baby.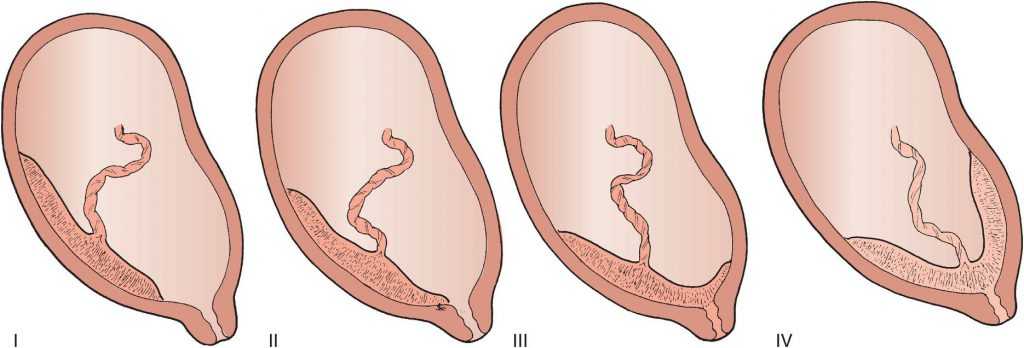 You can make an appointment with an obstetrician-gynecologist and choose a doctor – professor.
You can make an appointment with an obstetrician-gynecologist and choose a doctor – professor.
I’m 22 weeks pregnant, I was diagnosed with “Low Placental” on ultrasound. What does this mean for me and my baby?
A low placenta can cause placental insufficiency, premature termination of pregnancy, premature placental abruption, etc.
At 14 weeks, ultrasound diagnosed placenta previa, at 19 weeks, ultrasound said that there is no placenta previa, but there is a marginal attachment of it. What does this mean?
Your placenta has begun to “migrate”. At first, it completely covered the internal pharynx, now it only reaches it with its lower edge. With a good set of circumstances, one can hope that gradually the placenta will completely “rise”.
Pregnancy 15 weeks, according to the results of ultrasound: placenta along the anterior wall, 1.7 from the internal os, low location of the chorion. Is this normal or pathological?
Is this normal or pathological?
While this is a statement of fact. If after 20 weeks the placenta (chorion) does not rise, then low placentation will be considered as a pathology.
Pregnancy 23-24 weeks, ultrasound said that the uterus has increased tone and low placenta. The doctor prescribed Genipral and Verapamil. What is the likelihood that everything will be back to normal?
After the normalization of the uterine tone (for this you have been prescribed drugs), the placenta will most likely rise.
On ultrasound at thirteen weeks I was diagnosed with a low position of the placenta – 3.8 cm from the pharynx. How dangerous is it? How dangerous is air travel?
At 13 weeks of gestation, a distance of 3.8 cm from the edge of the placenta to the area of the internal os is absolutely normal. The danger of any airplane flight for a pregnant woman is the possibility of placental abruption and termination of pregnancy.